ORCID ID
Marta Setiabudy: https://orcid.org/0009-0006-4522-6259, Dewa Ayu Putri Sri Masyeni: https://orcid.org/0000-0003-1170-1841, Anak Agung Gede Indraningrat: https://orcid.org/0000-0002-8679-6016, I Ketut Agus Indra Adhiputra: https://orcid.org/0000-0002-3639-529X
Abstract
Highlights: 1. The significance of Staphylococcus aureus and coagulase-negative Staphylococcus, which are more likely to infect immunocompromised patients, needed to be researched in greater depth. 2. Coagulase-negative Staphylococcus was found to form significantly more biofilm than Staphylococcus aureus. 3. Wound care and changing medical devices in immunocompromised patients on a regular basis may provide benefits to prevent biofilm formation by Staphylococcus spp. Abstract Staphylococcus spp. are typically commensal microorganisms that can exist in the human body without causing illness. However, these bacteria have virulence factors, e.g., biofilm formation, that are important to note. Because biofilms shield bacteria from opsonophagocytosis and antimicrobial agents, they can cause persistent or chronic infections. Once they form biofilms, both Staphylococcus aureus and coagulase-negative Staphylococcus (CoNS) can potentially cause incurable infections. This study aimed to compare biofilm formation in Staphylococcus aureus and coagulase-negative Staphylococcus as a guide for the prevention and management of infection, which will maintain and improve the good health of the general population. This was an analytic research with a cross-sectional design. The study began by collecting the samples, identifying the species, and testing the biofilm production with a microtiter plate, which was then analyzed with an enzyme-linked immunosorbent assay (ELISA). Data analysis was conducted using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, N.Y., USA). Comparison tests were conducted using an independent t-test. A value of p<0.05 was used as the cut-off that indicated significance. The total samples were 36 clinical isolates, consisting of 18 Staphylococcus aureus and 18 coagulase-negative Staphylococcus. The specimens consisted of 20 blood samples (55.6%) and 7 wound swabs (19.4%). The biofilm test on the samples showed that 83.3% of the samples produced biofilms. The data revealed that the isolates formed biofilms, with 14 isolates (38.9%) in the strong category, 10 isolates (27.8%) in the moderate category, and each of 6 isolates (16.7%) in the weak and non-existent categories. Both Staphylococcus spp. appeared to have biofilm-forming activity, but coagulase-negative Staphylococcus appeared to be significantly more dominant (p=0.008). Strong biofilm was produced by 61.1% of coagulase-negative Staphylococcus isolates. In conclusion, coagulase-negative Staphylococcus formed a stronger biofilm than Staphylococcus aureus. Its presence as an infection-causing bacteria, particularly in immunocompromised patients, should not be underestimated.
Keywords
Biofilm, Staphylococcus, human and health, immunocompromised patients
First Page
222
Last Page
228
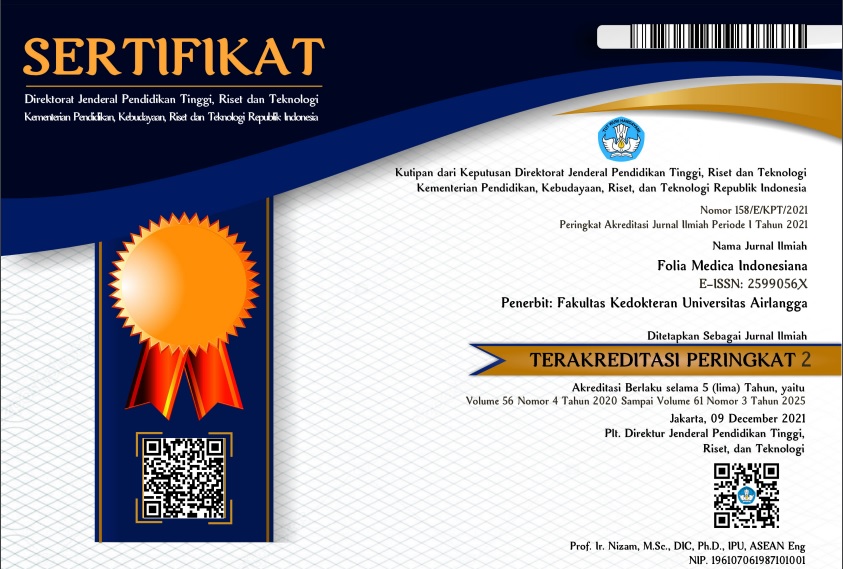
DOI
10.20473/fmi.v59i3.44598
Publication Date
9-10-2023
Recommended Citation
Setiabudy, Marta; Masyeni, Dewa Ayu Putri Sri; Indraningrat, Anak Agung Gede; Suryawan, Kadek; Adhiputra, I Ketut Agus Indra; and Rahman, Muhammad Amirul bin Abdul.
2023
Biofilm Formation in Staphylococcus aureus and Coagulase-Negative Staphylococcus.
Folia Medica Indonesiana. 59,
3 (Nov. 2024 ), 222-228.
Available at: https://doi.org/10.20473/fmi.v59i3.44598